Release date: 2014-05-23
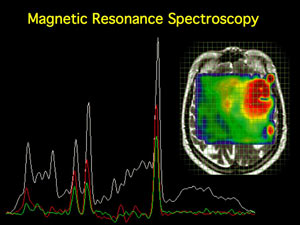
A study published in the Journal of the American Medical Association (JAMA Neurol. Published online May 19, 2014) showed that MR spectroscopy measurements can be used to predict the progression of disability progression in multiple sclerosis (MS).
The study showed that the ratio of inositol to nitrogen-acetylaspartate complex (mI:NAA) and secondary elevation of EDSS score, aggravation of brain atrophy and clinical disability for 12 months in apparent normal white matter There is a strong correlation between the deterioration progress.
Research details
A total of 59 patients and 43 healthy controls were included in the study, and a cohort of 220 was established to confirm the findings. The researchers found that the mI:NAA ratio is "a powerful cross-sectional predictor of decreased brain volume and clinical disability."
Given the impact of inter-individual differences on outcomes, the researchers themselves questioned whether this ratio could be applied to individuals at the clinical level. However, they also believe that the results of the study “are related to some of the more basic content of the disease progression process.â€
In this study, Pelletier and colleagues performed MR spectroscopy on exploratory samples and collected several parameters such as apparent normal white matter and gray matter NAA and mI, apparent normal white matter myelin water fraction (WMF). And conventional markers, including axonal injury, astrocyte proliferation, and demyelination.
Researchers say these indicators are not arbitrary. NAA is a component of neuronal cell bodies and axons. In MS patients, the level of this substance is reduced. As a component of astrocytes, mI levels are elevated in MS patients; WMF is related to myelin integrity. The index decreases with the demyelination process.
The results of the previous sample confirmed that the NAA level of apparent normal white matter was significantly decreased in MS patients compared with the control, and the apparent normal white matter or gray matter mI level was significantly increased. In addition, the MWF of these patients also decreased significantly, but the absolute value of the difference was not large (6%).
So far, the most significant difference between the MS group and the control group was the ratio of mI:NAA in the apparent normal white matter: MS patients were 31% higher than the control, while in the individual analysis, the difference did not exceed 19%.
During a 4-year clinical follow-up, this ratio was associated with brain atrophy: for every 1 point increase in this ratio, brain volume decreased by 1.7% per year (95% CI 0.3-3.0%); this ratio is not related to the EDSS score itself. However, it is related to another clinical measurement index, the MS function comprehensive score: for every 1 point increase, the score decreases by 0.52 points (95% CI 0.23-0.82).
In addition, validated samples enrolled in 220 MS patients showed the same trend during the 4-year follow-up period.
There are exceptions, however, that the apparent normal mI:NAA ratio is also significantly associated with changes in EDSS scores: for every 1 point increase in the ratio, the score increases by 0.57, 95% CI 0.015-1.13. However, this ratio is less predictive of changes in MS function scores: for every 1 point increase in the ratio, the score drops by 0.23 points, 95% CI 0.05-0.41).
Pelletier and colleagues also reported that for each standard deviation of the mI:NAA ratio, the odds ratio [OR] for sustained progression of EDSS within 12 months was 1.46 (95% CI 1.10-1.94). For the MS function score, this trend also exists, but it is not significant.
Perhaps because the study is biased toward basic science rather than dedicated to exploring clinical diagnostic tools, the researchers did not report possible thresholds for clinical prediction. Therefore, they did not conduct sensitivity-specific analysis for this ratio with other markers.
Expert point of view
In the editorial editorial, experts also showed a strong interest in this potential biomarker.
“The study is impressive, and the long-term biomarker of MS is entirely plausible,†said Dr. David H. Miller of University College London. He did not participate in the study.
"In a proof-of-concept study of MS neuroprotective therapy, the mI:NAA ratio can be considered as a prognostic measure," Dr. Miller added. However, he also pointed out that the implementation of this operation may be relatively complicated, requiring expert supervision and strict quality control measures.
He suggested that the marker should be validated by a multicenter study to rule out the potential impact of differences in readings between different devices.
Source: Imaging May Aid in Predicting MS Progression, by John Gever, Medpage Today, May 20, 2014
Source: Medical Pulse
Rechargeable Hearing Aid
Rechargeable Hearing Aid
Shenzhen Sunshine Technology Co.,Ltd , https://www.yatwinsz.com